Helicobacterpylori (H.pylori) is a kind of bacteria.unique, canPersistent colonization in human gastric mucosaAnd bacteria that can cause stomach infections.
Helicobacter pylori isgram-negativeSpiral, micro-aerobic bacteria inhabit human gastric mucosa. More than half of the people in the world are infected with Helicobacter pylori, but many of them have no clinical symptoms. Helicobacter pylori and its prevalence rate are as high as 80% in some people.
It is speculated that Helicobacter pylori may be a part of human indigenous microbiota, and it has a very complicated relationship with human hosts.
This paper mainly discusses how Helicobacter pylori co-evolved with human beings, and the possible mechanism can explain the positive and negative correlation between Helicobacter pylori infection and the development of several diseases in population-based research, as well as the respective results of how inflammation and/or microbial changes are related.
one
Symptoms and complications of Helicobacter pylori
Most people infected with Helicobacter pylori have no obvious symptoms, but when symptoms appear, they are generally the following:
Nausea, stomach pain or heartburn, abdominal pain aggravated on an empty stomach.
What kind of situation is likely to be infected with this bacterium?
Helicobacter pylori may spread through contact with saliva, vomit or feces of infected people, and it can also be infected by eating contaminated food or water.
Most people infected with Helicobacter pylori are inChildhood infectionYes.
Some factors may increase the risk of infection with Helicobacter pylori:
For example, living in a crowded space, without clean water, and living with people with Helicobacter pylori.
When do you need to see a doctor?
When you feel unusual stomachache or discomfort, especially persistent or recurrent stomachache;
Dysphagia;
Bloody, black or tarry feces;
Vomiting is bloody or looks like coffee grounds;
…
In the above situation, it is best to see a doctor.
(If you take antibiotics at will, the effect is not good and it is likely to bring antibiotic resistance.)
How to diagnose helicobacter pylori?
At present, the most common and affordable method isBreath detectionIt takes only a few minutes from the analysis to the result, which is simple and accurate.
gastroscopyGastroscopy also includes detection of Helicobacter pylori, because active tissues in the stomach can be taken for pathological examination.
Antibody examinationThrough blood test, to determine whether you have been infected with Helicobacter pylori and are currently infected.
Does helicobacter pylori cause complications?
Include ulcers, gastritis and stomach cancer.
ulcer About 10% patients with Helicobacter pylori will develop gastric ulcer (pain). This happens when Helicobacter pylori destroys the mucosa that protects the inner walls of the stomach and small intestine, and gastric acid can penetrate into the lining and cause damage.
Helicobacter pylori can cause more than 90% intestinal ulcers and 80% gastric ulcers.
Ulcer itself can also lead to serious complications:
? Internal bleeding Gastric acid or ulcer seeping into blood vessels may lead to bleeding.
? block An ulcer will prevent food from leaving your stomach.
? perforate The ulcer may penetrate deep into the stomach or intestinal wall.
? peritonitis Peritoneal inflammation (peritoneum) may occur when an ulcer causes infection or inflammation.
gastritis Gastritis is inflammation of gastric mucosa. Helicobacter pylori is at increased risk of suffering from this disease.
If gastritis is not treated, it may lead to serious blood loss and may increase the risk of illness.gastric cancerThe risk. Gastric cancer is the second most common cause of death in the world.
In addition, Helicobacter pylori infection is also related to other diseases, such as ischemic heart disease, type 2, anemia, adverse metabolic characteristics of obese subjects and insulin resistance.
2
Helicobacter pylori and microflora
Helicobacter pylori (Hp) infection will produce drastic changes in the gastric microenvironment, which will further affectGastric microfloraComposition, and may be related toChanges of intestinal microfloraRelated. May triggerIntestinal symbiotic homeostasisMajor changes, resulting in a new gastrointestinal balance.
At the same time, the therapeutic strategies used to eradicate Helicobacter pylori can regulate this physiological symbiosis, but it may also be the opposite, influenced by its characteristics.. Infection, diet, antibiotics and/or lifestyleWill interfere with this symbiotic relationship.
Interference of Helicobacter pylori infection on gastric microflora
Next-generation sequencing was used to study the human gastric microflora in gastric juice and biopsy samples. The results showed that there were many bacterial groups in the stomach, which mainly consisted of five phyla, includingActinomycetes, Bacteroides, Firmicutes, Clostridium and Proteus.. Helicobacter pylori infection has greatly changed the characteristics of gastric microflora.
A preliminary study reported that Helicobacter pylori colonization changed the gastric microflora,Reduce that diversity of microorganismsEradication of Helicobacter pylori can restore microbial diversity.
Helicobacter pylori can regulate gastric microenvironment by several mechanisms. By interfering with the expression of proton pump, Helicobacter pylori can regulate the acidity of gastric cavity, thus making the microenvironment compatible with microorganisms that usually cannot grow in the stomach.
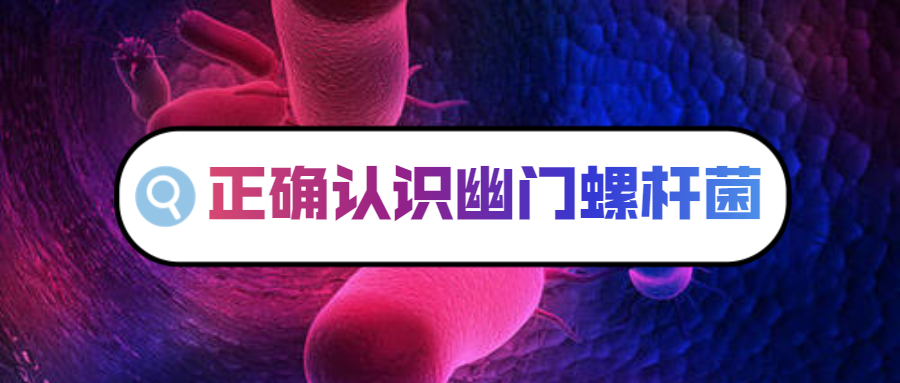
Study on evaluating the effect of Helicobacter pylori infection on gastric microflora

Tao et al., Helicobacter, 2020
In addition, the altered immune response due to the presence of Helicobacter pylori may affect other microbial groups. Helicobacter pylori may also change the growth of other microbial groups by mobilizing antibacterial peptides or by nutritional competition. In general, researchers have shown that,The colonization of Helicobacter pylori is related to the significant decrease of α diversity.. There is an inverse relationship between microbial diversity and Helicobacter pylori abundance.
Effect of Helicobacter pylori infection on intestinal microflora
Compared with the negative control group of Helicobacter pylori, individuals with a large number of Helicobacter pylori in the stomach have different intestinal flora, which indicates that there is interaction between gastrointestinal segments.
Most studies show that there is a positive correlation between Helicobacter pylori infection and intestinal microbial diversity. Because high microbial diversity is usually related to overall good health, it will be interesting to explore whether the increase of intestinal microbial diversity after Helicobacter pylori infection has some beneficial effects on the host.
Study on the influence of Helicobacter pylori infection on intestinal microflora

Tao et al., Helicobacter, 2020
There are significant differences in microbial community structure between Helicobacter pylori infection group and negative control group.
The composition analysis at the door level found that among the infected individualsThe abundance of Proteus increased significantly.This may be due to the transfer of Helicobacter pylori from stomach to intestinal cavity. It is worth noting that Bacteroides and Firmicutes (B:F) are similar.ratioexistIt is higher in helicobacter pylori positive group.The changed B:F ratio is related to the clinic, because it is found that Firmicutes and Bacteroides are related to the lipid metabolism and energy balance of the host.
Compared with the uninfected group,There was no significant difference in the abundance of Bifidobacterium, Lactobacillus and Ackermann mucilaginosus.. Other researchers have found that people infected with Helicobacter pyloriThe abundance of lactobacillus is higher..
A study found that among patients infected with Helicobacter pylori, the intestinal microflora of patients with atrophic gastritisStreptococcus is more abundant.
Another study found that individuals infected with Helicobacter pylori showedDecrease of short-chain fatty acid (SCFA) producers (such as butyrate)SCFA has a beneficial metabolic effect on the host.
In addition, given the widespread expression of SCFAs receptors in immune cells, these metabolites are considered to play an important role in regulating intestinal homeostasis. Therefore,Inhibition of SCFAs output during Helicobacter pylori infection may be harmful to human health..
Functional analysis shows that the disease-related pathway is more active among people with negative helicobacter pylori. In contrast, many metabolic pathways are over-represented in infected patients. Therefore, in the microbial community,Functional changes may be site specific.Yes, because the changes observed in the intestine are different from those observed in the stomach.Different trends.
Effect of eradication therapy on gastric microflora

Tao et al., Helicobacter, 2020
Sufficient evidence shows that the diversity of gastric microorganisms increased significantly after the successful eradication of Helicobacter pylori, but it did not improve after the failure of treatment. The researchers think it may take some time to recover, because they think the diversity increases gradually from week 0 to week 6 and week 26.
In addition, studies have shown that after the successful eradication of Helicobacter pylori,α diversity can be completely restored to the level of uninfected control group.. On the contrary, although the community structure can be partially restored after the eradication of Helicobacter pylori, there is controversy about whether there is still a significant difference between the eradication group and the negative control group.
Some researchers found that after two months of treatment, the composition of gastric microbial community recovered to the level of uninfected children. However, other studies confirmed that adult samples still showed different microbial structure after six months of successful treatment, but the negative control group was different.
Different age groups included in the analysis may explain the opposite conclusion, because another study of recruiting children also found that the flora structure of eradication group was close to that of Helicobacter pylori negative group after 4 weeks of treatment.
Evaluation of changes of gastric microflora after eradication therapy
Tao et al., Helicobacter, 2020
Component analysis revealed that the relative abundance of Helicobacter pylori decreased significantly after treatment, while other major bacteria, includingActinobacillus, Bacteroides, Firmicutes and Fusobacterium increased..
At the generic level, after treatment,Lactobacillus and Bifidobacterium(two recognized probiotics)The number has increased significantly..
The functional analysis of the two studies showed that after successful treatment,Protein and Up-regulation of Carbohydrate Metabolism Pathway. Therefore, during the period of Helicobacter pylori infection, the nutritional and metabolic function of gastric microflora is damaged, and eradication treatment can partially recover. However, the predicted functional changes need further verification.
Changes of intestinal microflora after eradication treatment
Proton pump inhibitors (PPIs) have been proved to have a significant effect on intestinal microflora by reducing acidity. Therefore, the effect of anti-Helicobacter pylori therapy on intestinal microflora is the joint result of PPIs, antibiotics and bismuth. The general trend is that,α diversity decreased immediately after eradication and then recovered..

Tao et al., Helicobacter, 2020
Specifically, how long the recovery will take remains to be clarified. Most studies have collected information within 2 months of follow-up.Decreased α diversityHowever, there is no significant difference between the report and the baseline.
However, a research report, from week 0 to week 6 and week 26,Sobs indexandChao indexAre falling, not statistically significant. Notably, another study found that,Different treatment optionsThe effects on intestinal microflora may be different.
In clinical trials, there are three different treatment schemes, including triple therapy, combined therapy and bismuth quadruple therapy. The results show that,The α diversity of all groups decreased at the second week., but only acceptThe patients with triple therapy only have basic α diversity at the eighth week.However, the α diversity of the other two groups after treatment.Can’t recover in a year..
It is hoped that future research will verify whether eradication therapy will lead to the continuous disorder of intestinal flora and how different treatment schemes affect reversibility.
Study on the influence of eradication therapy on intestinal microflora

Tao et al., Helicobacter, 2020
Probiotic supplementation can alleviate the diversity and structural disorder caused by antibiotics.
Probiotics have been proved to stabilize the microbial population and improve gastrointestinal symptoms. At the door level,Treatment for 6 monthsAfter observingThe thick-walled flora increased and Bacteroides decreased., indicating that it is observed in individuals infected with Helicobacter pyloriHigh B:F ratio reversal. Nine similar results were reported in another study.
Clinical evidence supports that obesity is related to the decrease of B:F ratio. Therefore, the decrease of B:F ratio detected in these studies may beWeight gain after eradication treatmentProvides a possible explanation. However, some researchers explain that,After 18 months of eradication, the reduced B:F ratio can be reversed.. Interestingly, probiotic supplementation has been shown to be associated with a higher B:F ratio after eradication therapy. It is worth noting that the results of the report are inconsistent.
A study showed that the B:F ratio increased immediately after treatment and remained above the baseline level at the 13th week. The classification map of metagenome research shows that,The relative abundance of Bifidobacterium decreased after treatment.. However, another study showed that Bifidobacterium increased after 6 months of successful eradication.
Enriched in the intestinal microflora of Helicobacter pylori positive atrophic gastritisStreptococcus decreased significantly after eradication treatment..
Although the long-term changes of intestinal microflora are different in different studies, it seems to be consistent to eradicate the short-term disorder that causes intestinal homeostasis.
Effect of eradication therapy on antibiotic resistance of intestinal flora
With the wide application of eradication therapy, the emergence of antibiotic resistance has become an important problem in clinical practice.
After the eradication of Helicobacter pylori infection, the increase of antibiotic resistance and the post-eradication treatmentLong-term security is an important issue..
Individualized treatment guided by drug sensitivity test can provide reliable and excellent eradication rate in first-line treatment, but it is expensive and not widely available. According to the antibiotic resistance in local areas,Empirical therapy for specific populationIt may be an alternative strategy.
three
Host and environmental determinants of helicobacter pylori-related diseases
Has been shown to change the risk of helicobacter pylori-related diseasesHost factorIncluding the hostageThe duration between the acquisition of Helicobacter pylori and Helicobacter pylori infection, but more importantly, the host.Immune mediator(polymorphism) andAcid secretion state.
In addition to host factors,Smoking and dietEnvironmental factors will also affect the niche of Helicobacter pylori colonization, so it may affect the disease risk.

Karin et al., FEMS Microbiol Rev. 2006
Age
existAt a young ageInfection with Helicobacter pylori increases the risk of gastric ulcer and gastric cancer. The development of gastric ulcer and gastric cancer requires long-term infection of Helicobacter pylori, so it is speculated that these diseases are more common in patients with chronic infection of Helicobacter pylori.
In addition, this association is considered to be caused byDifference of host immune response in different age groupsDecided by.
inflammatory mediator
After being infected with Helicobacter pylori, the host gastric epithelial cells release cytokine IL-8. This cytokine is involved in the recruitment of macrophages, neutrophils, mast cells, B cells and T cells to the inflammatory site. These cells further enhance the immune response by secreting other inflammatory mediators, such as interferon-G, tumor necrosis factor-A and interleukin-1B.
Schematic diagram of pathogenesis related to Helicobacter pylori

Karin et al., FEMS Microbiol Rev. 2006
A) In human stomach, Helicobacter pylori mainly colonizes the antrum lacking gastric acid secretion wall cells;
B) In gastric pits, Helicobacter pylori proliferates especially near the tight junction of epithelial cells;
C) Helicobacter pylori plays an important role in colonization, persistence and disease development.
The immune response to Helicobacter pylori is further manifested in activated human neutrophils.Oxidation explosion. This outbreak will lead to the release of reactive oxygen species (ROS), which is a low molecular weight metabolite that can destroy important biological components including nucleic acids. ROS mayDamage genes that control cell growth; And stimulate the development of cancer. Therefore, the existence of immune mediators will lead to gastric epithelialImpaired integrity. This kind of injury is the cause of most pathology related to Helicobacter pylori infection, rather than direct Helicobacter pylori activity.
Immune cells existing during Helicobacter pylori infection are mainlyProinflammatory cellInstead of anti-inflammatory cells. Pro-inflammatory mediators are secreted by helper T cells 1(Th1). Primitive T cells are driven by many factors to differentiate into Th1 cells, such as TNF-a and IL-12.
Stimulated by Helicobacter pylori, monocytes produce a large amount of cytokine IL-12. Therefore,By stimulating the release of IL-12, Helicobacter pylori enhances the pro-inflammatory response.. This leads to more damage to the gastric epithelium, which is easy to develop gastric atrophy.
Some host genes encoding immunoregulatory factors contain polymorphic regions. These genesPolymorphism will change their transcription, thus affecting the inflammatory process. Therefore, the risk of Helicobacter pylori-related diseases may change. So far,Polymorphism of IL-1b, IL-1 receptor antagonist, IL-10 and TNF-a genesHas been proven to be related to the remote endGastric cancer is significantly related..
Human leukocyte antigen (HLA) helps to eliminate pathogens by presenting peptide fragments derived from pathogens to appropriate T cells. HLA gene is highly polymorphic, and someHLA alleles are related to the occurrence of gastric adenocarcinoma..Helicobacter pylori infection is also related to the occurrence of gastric adenocarcinomaBut its existence has nothing to do with the existence of these HLA alleles. Therefore, the importance of HLA alleles in Helicobacter pylori-mediated adenocarcinoma is still controversial.
Therefore, genetically predeterminedDominant pro-inflammatory Th1 response is associated with Helicobacter pylori disease..
On the other hand, the intensity of Th1 response may be limited by the production of anti-inflammatory Th2 cytokine IL-10, thusProlonging infection time. Th2 type reaction is caused by parasites. Therefore, the inflammatory reaction and pathological changes of people infected with Helicobacter pylori gradually weaken. This may lead to these individualsTime delay of progression from chronic gastritis to gastric cancer. In addition, different pro-inflammatory reactions may directly lead to different pathways of Helicobacter pylori-related pathology.
Gastric acid secretion
Th1 reaction mentioned above causes gastric parietal cells to inhibit their acid secretion. The environment with low acidity may promote the spread and persistence of Helicobacter pylori. In addition, whenGastric acid level is low.Microorganisms other than helicobacter pylori may grow in the human stomach, thusEnhance local inflammatory response.Pro-inflammatory cytokineandDecreased gastric acid secretionJoint action ofincreaseThe patients suffering from peptic ulcer and gastric cancerrisk.
On the other hand, when the secretion of acid decreases, duodenal ulcer is unlikely to occur. When the secretion of acid is enhanced, the risk of duodenal ulcer increases. However, it is alsoLow acidityUnder the conditions,The risk of duodenal ulcer may increase after Helicobacter pylori infection..
Gastric parietal cells control itAcid-producing abilityIt is important in the development of helicobacter pylori-related diseases. Helicobacter pylori infection mainly occurs in human stomach.Weakly acidic parts, such as the gastric antrum. Therefore, the host with high gastric acid secretion has a high density of Helicobacter pylori in the gastric antrum, and it mainly develops intoGastric antral gastritis. Subsequently, the intact parietal cells in the stomach are stimulated to secrete acid, thus inducing gastric metaplasia of the duodenum. Helicobacter pylori colonizes this gastric metaplasia, which may lead to duodenal ulcer.
On the other hand, the host with low gastric acid secretion is not only susceptible to Helicobacter pylori infection in gastric antrum, but also susceptible to Helicobacter pylori infection in gastric body. The infected Helicobacter pylori can further inhibit the acid secretion of gastric parietal cells. This can stimulate the continuous proliferation of gastric epithelial cells, leading toProgressive loss of gastric glands, eventually leading to gastric atrophy and cancer.
Environmental determinants
smoke
Some environmental factors are related to the pathogenesis of Helicobacter pylori. Smoking is the main factor in the development of gastric cancer. Tobacco smoke contains carcinogenic nitrosamines, which leads to the development of cancer.
High salt diet
Some dietary factors are related to helicobacter pylori disease. High-salt diet is associated with the increased rate of Helicobacter pylori colonization, gastritis and gastric cancer risk. High salt concentration leads to atrophy of parietal cells and destruction of mucosal barrier. However, only long-term high salt intake will increase the risk of Helicobacter pylori-related diseases.
High rice intake
There is a positive correlation between high rice intake and gastric cancer. Rice contains carbohydrates, which may irritate the gastric mucosa.
Low intake of fruits and vegetables
Low intake of fruits and vegetables may increase the risk of gastric cancer. Fruits and vegetables contain antioxidants vitamin C and beta-carotene, which can prevent cancer by neutralizing active oxygen.
Therefore, although several environmental factors are considered to be related to the occurrence of Helicobacter pylori-related diseases, their roles are often controversial. It is speculated that different environmental factors and the complex interaction between host and bacterial factors hinder the interpretation of the research results.
four
Bacterial determinants of helicobacter pylori infection
The overall influence of Helicobacter pylori factors in the development of diseases is complicated. Up to now, several specific proteins of Helicobacter pylori related diseases have been described. These protein are believed to be the reason for the persistence of Helicobacter pylori. As a side effect, these Helicobacter pylori proteins induce and change the inflammatory process and damage the gastric epithelium, thus determining the outcome of Helicobacter pylori infection.
CagA
Compared with patients infected with cagA-negative Helicobacter pylori isolates, the colonization of Helicobacter pylori isolates carrying cytotoxin related gene A(cagA) is similar to that of patients infected with CagA-negative Helicobacter pylori isolates.The risk of severe gastritis, peptic ulcer and distal gastric adenocarcinoma is increased.Related.
The presence or absence of cagA gene of Helicobacter pylori is often used as a marker for the presence or absence of PAI in Helicobacter pylori. Cag PAI consists of about 30 genes and accounts for 50%-70% of all Helicobacter pylori isolates. The recombination between two 31 bp repeats flanking cag PAI may lead to the deletion or acquisition of the whole cag region.
The 18 genes on cag PAI are very important to the development of CAG PaiIt is very important to produce type IV secretion system.. Type IV secretion system transports proteins (related to virulence) in bacterial cells to the cytosol of host cells. This usually leads toInitiation of cascade reaction of epithelial cell reactionFor example, changes in cytoskeleton and secretion of cytokine IL-8.
In Helicobacter pylori, the components of type IV secretion system transport CagA protein to gastric epithelial cells. Subsequently, CagA protein was phosphorylated. Then, this phosphorylated CagA interacts with the host phosphatase SHP-2, causing the rearrangement of cytoskeleton. This leads to morphological changes of host cells, also known as "hummingbird" phenotype. PhenotypicCharacterized by cell diffusionProlonged growth of epithelial cells and the existence of platelet lipoprotein and filamentous pseudopodia.
As a counteracting event, phosphorylated CagA interacts with host Src kinase, thus weakening the signal transduction of host SHP-2 phosphatase. This process reduces the rearrangement of cytoskeleton andPrevents further phosphorylation of CagA..
Recently, it has been proved that Helicobacter pylori strains induce a high level of CagA phosphorylation in vivo. Epithelial cells induce more cytoskeleton changes, which are more likely to be related to gastric cancer.Difference of phosphorylation level of CagAIt is composed of tyrosine phosphorylation motifs (TPM) in 30 regions of cagA gene.Difference in quantityCaused.
Helicobacter pylori population needs minimal immune recognition. Therefore, in the shrinking niche, theseThe subclones with reduced TPM number induced a weak host immune response..
On the other hand, higher levels of CagA phosphorylation can cause stronginflammatory reaction. This kind of inflammation will lead to atrophy and may play a role in niche acid stress that limits high acid output.
Through observation, it was found that Helicobacter pylori strains lacking cagA gene were isolated from patients with peptic ulcer or gastric cancer, although their frequency was lower than that of cagA-positive Helicobacter pylori strains.
The association between cagA and Helicobacter pylori-related diseases is different in different geographical areas. This variation may be related to the difference of CagA expression.
However, CagA is not unique. Helicobacter pylori protein is responsible for barrier dysfunction, and this process is not lost with the clearance of CagA. VacA protein discussed in the next section is also important.
VacA
It is initially shown that eukaryotic cells undergo vacuolation and continuous degeneration in an in vitro test system with Helicobacter pylori. It turned out that this phenomenon was caused byHelicobacter pylori toxinInduced, now known as vacuolar cytotoxin A(VacA).
VacA or CagA alone cannot be used as a determinant of clinical outcome.
How does VacA function and lead to cell death?
Helicobacter pylori VacA is a highly immunogenic 95-kDa protein. VacA binds to the apical part of epithelial cells to form anion selective pores.
Through these holes,Bicarbonate, chloride and ureaReleased from the cytoplasm, VacA is then endocytosed into the late endosomal compartments and changes the permeability of these compartments.
In the presence of weak alkali (such as ammonia), this will lead to the influx of water, which will lead to vesicle swelling and vacuole formation. intra-cellularInjury of endocytosis pathwayEventually lead tocell death.
This leads to the decrease of epithelial cell resistance, so low molecular weight molecules such as Fe3+ and Ni2+ can easily pass through the epithelial cell layer.Fe3+ and Ni2+ molecules are the key factors of Helicobacter pylori growth and urease activity, respectively..
Therefore, it is speculated that Helicobacter pylori can obtain these key factors more easily by degrading the epithelial cell barrier.
Helicobacter pylori VacA alsoRelated to the degradation of parietal cellsThis leads to a decrease in acid secretion, making it easier for the host.Suffer from stomach cancer. Difference of VacA expression level during persistent infectionLead to toxicity change. Therefore,The growth and decline of ulcer can be explained by the change of VacA expression with time..
The transcription of vacA gene was induced near gastric epithelial cells in vitro. This discovery confirms the importance of interaction between VacA and host cells. In addition, VacA canEscape adaptive immune response, thusEnhance the persistence of helicobacter pylori in gastric mucus layer.
Helicobacter pylori outer membrane protein (HOPs)
Among gram-negative bacteria,The outer membrane mediates the interaction with its surroundings.. During infection, it is assumed that the protein existing on the outer membrane of Helicobacter pylori is changed, so that the recognition function of the host immune system is minimized.
Helicobacter pylori isolates contain about 30 different outer membrane proteins (Hops). Several of them are adhesins. In gram-negative bacteria, adhesin most often forms the structure of polymeric fimbriae. However, in Helicobacter pylori, theseAdhesion has adapted to the gastric environment., in whichAcidic conditionIt may make this polymer fimbriae structuredepolymerization.
Fucoid glycosylatedglycoproteinAnd sialylatedglycolipidHave been proved to be helicobacter pylori in gastric epithelium.Binding site.
Adhesion to host cells can protectHelicobacter pylori is protected from peristalsis and mucosal shedding..
In addition, it is speculated that adhesion can make Helicobacter pylori better obtain nutrients released from gastric epithelium, and it is moreEffectively deliver bacterial toxins to host cells..
On the other hand, at the site of severe inflammation,Loss of adhesion characteristicsIt may make helicobacter pyloriEscape the killing of host immune cells.So far, some hops are related to the development of diseases.
Helicobacter pylori BabA (HopS) mediates the adhesion of Helicobacter pylori to human Leb blood group antigens, which exist in gastric epithelial cells. BabA adhesion promotes the colonization of Helicobacter pylori and increases the secretion of IL-8 by epithelial cells, resulting inIncreased mucosal inflammation.
Both mechanisms of BabA regulation are helpful to promote the dynamic response of chronic infection.
During chronic inflammation, all types of Leb binding can be obtained in all blood groups by choosing to increase or decrease the adhesion period.
The glycosylation pattern of host mucosa leads to the evolution of BabA, which adapts Helicobacter pylori strains to their individual hosts, whichHelps avoid host reactions.And cause helicobacter pylori infection worldwide.Abnormal long-term.
Virulence factors of Helicobacter pylori plasticity region
The comparison of the genome sequences of two isolated strains showed that about 6%-7% of Helicobacter pylori genes in one strain did not exist in the other strain, and vice versa.
About half of the strain-specific genes exist in hypervariable regions; Plastic zone. Genes located in this plastic region usuallyAssociated with increased virulence.
In helicobacter pylori, the plastic region doesencodeRelated to type IV secretion.Vir ATPase. In Helicobacter pylori, this secretion system is important in, for example, secreting CagA cytotoxin. So far, some helicobacter pylori located in the plastic zonegeneAnd helicobacter pyloriRelated diseasesRelated.
Helicobacter pylori Jhp0947 and Jhp0949 are related to duodenal ulcer disease. These two genes are located in the plastic region of Helicobacter pylori strain J99, which is mediated by Helicobacter pylori.IL-12 releaseIt’s very important.
Extracted from monocytes in an in vitro test system. Cytokine IL-12 is essential to bias the immune response to pro-inflammatory Th1 response, and it is closely related to the formation of duodenal ulcer.
byjhp0947andjhp0949The function of the coded protein is unknown. However, it has been assumed that these proteins induce the production of pro-inflammatory cytokine IL-12 through interaction with monocytes.
The level of IL-12 increased.Will lead to the differentiation of naive T cells into activated Th1 cells, which will lead toIncreased inflammatory response and increased tissue damage..
HpJhp0950, which encodes a protein with unknown function, is also a part of J99 plasticity region. The existence of this gene is related to cagA, cagE, vacA s1m1, babA2, hopQ T1 and oipA.
Jhp0950 is adjacent to Jhp0949 in the genome of Helicobacter pylori J99. Unlike Jhp0949, Jhp0950 is not associated with an increased risk of duodenal ulcer. However, its association with disease supportsHelicobacter pylori gene located in plastic region may be related to toxicity.The point of view.
Other virulence factors of Helicobacter pylori
In the United States and the Netherlands, helicobacter pylori iceA1 gene (one of the two allelic variants of iceA gene) is infected by helicobacter pylori.peptic ulcerIn patients with helicobacter pylori infection.Gastritis patientIt is more common.
Similar to many other virulence-related genes, the relationship between IceA expression and Helicobacter pylori-related diseases is as followsGroup dependenceYes.
In Southeast Asia, there is no correlation between iceA1 and Helicobacter pylori-related diseases. Interestingly, the Helicobacter pylori isolated from South Africa which was positive for iceA1 was infected by Helicobacter pylori.gastric cancerAmong patientsThan only inHelicobacter pylori infectedIt is more common in patients with gastritis.
Note: Helicobacter pylori iceA1 was originally identified after being exposed to gastric epithelial cells. The endonuclease encoded by iceA1 gene is very similar to restriction endonucleases NlaIIIR in Lactococcus, and the highly conserved activity of deoxyribonucleic acid adenine methyltransferase encoded by Helicobacter pylori seems to be related to the control of gene expression of Helicobacter pylori.
Helicobacter pylori Jhp1462 is associated with an increased risk of MAL T lymphoma, duodenal ulcer and gastric adenocarcinoma. The function of protein encoded by Jhp1462 is unknown, and its importance in the development of severe gastroduodenal diseases remains to be clarified.
Above, we can see that Helicobacter pylori has brought various adverse effects to the human body in various ways. It seems that it should not survive in the human body for a long time. However, Helicobacter pylori has a long history in the human body.So how does Helicobacter pylori protect itself and survive in the human body?
five
Determinants of Helicobacter pylori colonization and persistence
Before the disease occurs, Helicobacter pylori willLong-term infection of human gastric mucosa. Therefore, the factors leading to the colonization and persistence of Helicobacter pylori and the pathogenesis related to Helicobacter pylori are as followsinner link. After entering the gastric cavity, Helicobacter pylori must cope with gastric acid.
Helicobacter pylori passes through itacid resistanceSurvive in this acidic condition: then pass through the mucus layer to reach its position close to the gastric epithelial cells. Chemotaxis, motility and adhesion are important processes of gastric epithelial cell colonization.
In order to persist in human gastric mucosa for a long time, Helicobacter pylori still needs nutrition from its host. This is achieved by degrading the integrity of the mucous layer and the underlying gastric epithelial cells. In addition, throughInhibition of host immune system, antigenic variation and antigenic mimicryThe elimination of helicobacter pylori is avoided.
acid resistance
The lower pH value of helicobacter pylori growth is5.0-5.5Depending on the isolate being tested. In the gastric mucosa, the pH is also acidic, varying from 4 to 6.5. Moreover, when the mucus layer is destroyed, the pH value may drop occasionally.
Survival of Helicobacter pylori after acid shock (pH<3)Depending on the urease activity of Helicobacter pylori proteinThe enzyme converts urea into ammonia and bicarbonate. This causes the periplasm or cytoplasm of Helicobacter pylori to be neutralized. Urease activity of helicobacter pylori is important for survival in vitro at acidic pH and in animal modelsColonization of gastric mucosaIt is very important, which proves the importance of urease in Helicobacter pylori infection.
At neutral pHThe combination of highly active urease and acid-regulated urea channelsIt explains why the viability of Helicobacter pylori in human stomach is unique. Effective inhibition of UreI protein will provide a method to eradicate Helicobacter pylori from normal, acid-secreting stomach.
Besides acid resistance, urease also has other basic functions related to gastric colonization.
Although urease is essential for the survival of acid shock, Helicobacter pylori urease is not enough to deal with chronic acidic environment near gastric epithelial cells. useacid inhibitorTreatment could not restore the colonization ability of urease negative mutant in the stomach of dwarf piglets.
Urease participates in nitrogen metabolism of Helicobacter pylori.Ammonia and bicarbonate produced by urease activity are considered to affect many cellular processes in the host, including cell lysis.
In addition to urease,Non-urease genes also contribute to acid resistance.And the survival and growth at acidic pH have nothing to do with urease. Among these non-urease genes, three regulatory proteins (Fur, NikR and HP0166) have been shown to contribute to the adaptability of Helicobacter pylori. This shows the importance of strictly adjusting the acid resistance mechanism.

Karin et al., FEMS Microbiol Rev. 2006
NikR directly and indirectly regulates the expression of urease through Fur regulation system. CsrA regulates the expression of Fur and HspR regulatory systems. Through the interaction of different gene regulatory proteins, Helicobacter pylori can sense and respond to a variety of signals.
Chemotaxis and movement of cells
The gastric epithelial cell layer is covered with a thick layer of mucus. It is assumed that this layer is relatively impermeable even to small molecules. Helicobacter pyloriInitiative and chemotaxisIs effective in penetrating this mucus layer.key.
In the mouse infection model, almost any mutation of motor and chemotactic system genes eliminated the ability of Helicobacter pylori to infect gastric mucosa, and emphasized the importance of these factors to colonization.
motility
The motility of helicobacter pylori is through the existenceTwo to six polar sheathed flagellaAnd realized it. Flagella consists of three structural elements: matrix, hook and filament. Up to now, more than 50 species of protein are related to the structure or regulatory organization of flagella.
Flagella filament consists of two subunits FlaA and FlaB. FlaA and flaB mutants of Helicobacter pylori could not be colonized in the model of infected piglets, indicating that Helicobacter pyloriFlagella is necessary for colonization.The virulence of Helicobacter pylori is also increased.
The motB gene of Helicobacter pylori encodes the flagella motor rotation protein. Helicobacter pylori motB gene knockout mutant still contains flagella, but it can’t move. The ability of the mutant to colonize mice decreased, which confirmed thatExercise is necessary for complete infectivity..
The regulation of flagella gene transcription is different from many other bacteria. Contrary to many other gram-negative bacteria with flagella, Helicobacter pylori has no transcription regulator to regulate the transcription of flagella gene.
It is speculated that the movement of Helicobacter pylori does not need strict regulation, because it is indispensable at any time. However, some transcriptional regulation can still be seen in Helicobacter pylori. For example, FlhA and FlhF in protein, the components of the matrix, need to appear before the transcription of flagella genes in the middle and late stages.
chemotaxis
In addition to mobility, chemotaxis is also essential for the colonization of Helicobacter pylori. Chemotaxis allows Helicobacter pylori to direct its movement to the gastric epithelial layer.
The chemotactic receptor sensor of Helicobacter pylori encoded by HP0099 recognizes bicarbonate and arginine as attractants. This sensor protein on the outer membrane of Helicobacter pylori is similar to that on the outer membrane of Helicobacter pyloriReaction regulator CheYCoupling.
CheY, a reaction regulator, regulates the expression of flagella motor protein and makes Helicobacter pylori swim to its niche.
A knock-out mutant of response regulator CheY failed to colonize in abiotic piglets, which emphasized thatThe Importance of Chemotaxis in Initial Colonization.
The knock-out mutant of CheY and its histidine kinase showed thatChemotactic response to mucin is weakened..
Immune evasion
In the long-term colonization process, the host has a strong immune response to a variety of Helicobacter pylori antigens. However, these antigens are usually not exposed on the surface.
On the other hand, the antigens exposed on the surface are usually highly diverse, which makes it more difficult for the host to eliminate Helicobacter pylori. Helicobacter pylori infection rarely produces enough immune response to remove bacteria. In fact, Helicobacter pylori canEffectively avoid innate and adaptive immune responses..
The innate immune response can’t recognize Helicobacter pylori substantially. Escherichia coli lipopolysaccharide (LPS) activates innate immune response through TLR4. However, Helicobacter pylori LPS is far from being an effective inducer of gene expression mediated by TLR4.
In Helicobacter pylori, the activation efficiency of immune response mediated by TLR5 is also low. Compared with Salmonella enterica serotype typhimurium flagellin, Helicobacter pylori flagellin is not released, and it is not so strong in activating IL-8 secretion through TLR5.
The failure of innate immune response to recognize Helicobacter pylori may lead to the failure of adaptive immune response to subsequently clear the infection.
The escape of adaptive immune system is mediated by at least two important mechanisms:Antigen simulationandimmunosuppression. Antigen simulation leads to the host immune system can not correctly identify Helicobacter pylori. For example, the Le blood group antigen on Helicobacter pylori LPS is also expressed on human epithelial cells. As a result, the immunogenicity of Helicobacter pylori LPS is poor, which supports the persistence of Helicobacter pylori. The ability of Helicobacter pylori strains lacking O antigen on their LPS to colonize mice was significantly reduced. Therefore,The typical structure of Helicobacter pylori LPS is very important in colonization..
In addition to avoiding immunity through antigen simulation,Immunosuppression also contributes to the chronic infection of Helicobacter pylori..
The immune response may be biased towards a more anti-inflammatory response or down-regulated (VacA). VacA of Helicobacter pylori can block the fusion of phagocyte and lysosome in macrophages, so that macrophages cannot kill Helicobacter pylori.
In addition, VacA expression blocks T cell activation and therefore proliferation, activates T cell apoptosis, and inhibits antigen presentation in T cells.
The antigen processing of B lymphocytes may be prevented, possibly by limiting the maturation of endosomes to MHC class II compartments where antigen loading occurs. Therefore,VacAT cell and B cell responses to Helicobacter pylori are limited..
The existence of Helicobacter pylori can prevent some diseases?
Through the above methods, Helicobacter pylori can survive in the human body. To some extent, Helicobacter pylori is not always harmful to human hosts.
Studies have shown that the existence of Helicobacter pylori may inhibit the bacteria that cause tuberculosis (Mycobacterium tuberculosis) and prevent asthma, Crohn’s disease, esophageal reflux, diarrhea and esophageal cancer. The decline in the incidence of Helicobacter pylori is related to the increase in the incidence of allergic diseases, autoimmune diseases, multiple sclerosis and abdominal diseases in children.
Therefore, to some extent, Helicobacter pylori has its existence value. This has caused a discussion about whether it is necessary to eradicate Helicobacter pylori.
06
Is it necessary to eradicate Helicobacter pylori?
It needs to be clear that Helicobacter pylori infection will not immediately cause fatal harm and serious consequences to human body, and the diseases caused by chronic gastritis, digestive tract ulcer and gastric cancer are the result of long-term existence and chronic interaction with other factors.
The fifth national consensus report on the treatment of Helicobacter pylori infection has the following statements:
The benefits of eradicating Helicobacter pylori vary among different individuals.
Eradication of Helicobacter pylori promotes the healing of peptic ulcer and reduces the incidence of ulcer complications. Eradication of Helicobacter pylori can alleviate about 80% of early gastric MALT lymphoma. Compared with the patients infected with Helicobacter pylori without symptoms and complications, the benefits of eradicating Helicobacter pylori in these patients are obviously greater. Individuals with high risk of gastric cancer include family history of gastric cancer, early gastric cancer after endoscopic resection, gastric mucosal atrophy and/or intestinal metaplasia. The benefit of eradicating Helicobacter pylori in preventing gastric cancer is higher than that of low-risk individuals.

Helicobacter pylori-related dyspepsia must be ruled out before a reliable diagnosis of functional dyspepsia can be made.
Helicobacter pylori gastritis patients with dyspeptic symptoms, eradication of Helicobacter pylori can make some patients’ symptoms get long-term relief, which is the preferred choice.
Helicobacter pylori infection is the main cause of peptic ulcer. No matter whether the ulcer is active or not and whether there is a history of complications, Helicobacter pylori should be detected and eradicated.
…
Generally speaking, for individuals who have no competitive factors (old age, co-existing diseases, community reinfection rate, health and economic factors, etc.), eradication of Helicobacter pylori treatment.The advantages outweigh the disadvantages.
Children:
Routine detection of Helicobacter pylori in children under 14 years old is not recommended. It is recommended to detect and treat Helicobacter pylori in children with peptic ulcer, and it is recommended to detect and treat Helicobacter pylori in children undergoing endoscopic examination due to indigestion.
Compared with adults, children’s eradication treatment has many unfavorable factors, including small choice of antibiotics and low tolerance to adverse drug reactions. In addition, children with Helicobacter pylori infection have a certain spontaneous clearance rate, and the reinfection rate after eradication may be higher than that of adults.
Older people:
The risk of adverse drug reactions in the treatment of helicobacter pylori eradication in the elderly is increasing, so the treatment of helicobacter pylori eradication in the elderly should be evaluated comprehensively and treated individually.
Questionnaire survey shows that most clinicians tend to be conservative about the treatment of eradicating Helicobacter pylori in the elderly. Generally speaking, the tolerance and compliance of the elderly (over 70 years old) to the therapeutic drugs for eradicating Helicobacter pylori are reduced, and the risk of adverse antibiotic reactions is increased; On the other hand, the potential benefit of eradicating Helicobacter pylori in patients with non-atrophic gastritis or mild atrophic gastritis to prevent gastric cancer decreased.
It is very important to treat the consequences of Helicobacter pylori infection reasonably, and whether it is necessary to intervene Helicobacter pylori infection in natural population needs to weigh the advantages and disadvantages comprehensively. For patients with eradication indications, standardized treatment is needed to improve the first eradication rate and reduce the occurrence of drug resistance.
07
Conclusion
In the process of chronic infection, many strains are colonized in one host at the same time, and the genetic variation of Helicobacter pylori isolates makes it difficult to predict the pathogenesis of Helicobacter pylori from a single factor. The co-evolution of Helicobacter pylori and its host enables it to settle for life.
With the improvement of modern health environment and the extensive use of antibiotics, the growth and spread of Helicobacter pylori is becoming more and more difficult, and the infection rate among the younger generation is low, and the infection rate of Helicobacter pylori will further decline in the next few decades.
A better understanding of the dialogue between Helicobacter pylori and other gastrointestinal microflora may provide a new direction for preventing or treating its infection.If helicobacter pylori infection is found in the health test report of intestinal flora, it should be paid attention to.When treatment is needed, new treatment strategies and drugs should be evaluated, or alternative strategies should be formulated to control the virulence of bacteria, so as to avoid ulcers and gastric cancer without eliminating its positive effects.
Appendix: Discovery History of Helicobacter Pylori
In the early 1980s, Helicobacter pylori was first discovered as the cause of stomach diseases. This discovery helps researchers to associate Helicobacter pylori infection with gastritis, ulcer and gastric cancer.
In 1982, two Australian researchers, Barry Marshall and Robin Warren, described the role of Helicobacter pylori infection.
However, Warren and Marshall’s theory about the function of Helicobacter pylori was not immediately accepted by the medical community. At that time, most scientists didn’t believe that bacteria could live in human stomach.
Marshall could not further test his work in laboratory mice, nor was he allowed to conduct experiments on people. Marshall, a brave scientific researcher, thought of a way.
He decided to eat Helicobacter pylori himself. He extracted the bacterium from the patient’s intestine, put it in the broth and drank it.
A few days later, Marshall developed intestinal symptoms, such as nausea, vomiting, bad breath and fatigue. He had a gastric biopsy and was able to culture Helicobacter pylori, which proved that bacteria caused his symptoms.
The medical community finally accepted the idea that Helicobacter pylori causes ulcers and other intestinal problems, but the obstacles to acceptance were long.
In 1994, the consensus development meeting of the National Institutes of Health officially recognized the close relationship between Helicobacter pylori and ulcers. The group suggested antibiotic treatment for patients with ulcers.
In 1996, FDA approved the first antibiotic therapy for ulcer caused by Helicobacter pylori.
A year later, the Center for Disease Control and Prevention (CDC) launched a national campaign in cooperation with other government agencies and academic institutions to provide doctors and patients with information about the relationship between Helicobacter pylori and ulcers.
In 2005, Marshall and Warren won the Nobel Prize in Physiology or Medicine. Ulcer is no longer regarded as an incurable chronic disease, but a disease that can be treated by short-term antibiotics and acid secretion inhibitors.
[References]
Burucoa C, Axon A. Epidemiology of Helicobacter pylori infection. Helicobacter. 2017 Sep; 22 Suppl 1. doi: 10.1111/hel.12403. PMID: 28891138.
Camilo V, Sugiyama T, Touati E. Pathogenesis of Helicobacter pylori infection. Helicobacter. 2017 Sep; 22 Suppl 1. doi: 10.1111/hel.12405. PMID: 28891130.
Eusebi LH, Zagari RM, Bazzoli F. Epidemiology of Helicobacter pylori infection. Helicobacter. 2014 Sep; 19 Suppl 1:1-5. doi: 10.1111/hel.12165. PMID: 25167938.
Mentis A, Lehours P, Mégraud F. Epidemiology and Diagnosis of Helicobacter pylori infection. Helicobacter. 2015 Sep; 20 Suppl 1:1-7. doi: 10.1111/hel.12250. PMID: 26372818.
Thorell K, Lehours P, Vale FF. Genomics of Helicobacter pylori. Helicobacter. 2017 Sep; 22 Suppl 1. doi: 10.1111/hel.12409. PMID: 28891132.
Julie Marks.Robert Jasmer, MD What Is H. Pylori? Symptoms, Causes, Diagnosis, Treatment, and Prevention. 2020.9
History of H. Pylori: What We Do and Don’t Know Before the discovery of the bacterium, doctors thought stomach ulcers were due to stress and spicy foods.
Burucoa C, Axon A. Epidemiology of Helicobacter pylori infection. Helicobacter. 2017 Sep; 22 Suppl 1. doi: 10.1111/hel.12403. PMID: 28891138.
Kamboj AK, Cotter TG, Oxentenko AS. Helicobacter pylori: The Past, Present, and Future in Management. Mayo Clin Proc. 2017 Apr; 92(4):599-604. doi: 10.1016/j.mayocp.2016.11.017.
Eusebi LH, Zagari RM, Bazzoli F. Epidemiology of Helicobacter pylori infection. Helicobacter. 2014 Sep; 19 Suppl 1:1-5. doi: 10.1111/hel.12165. PMID: 25167938.
Yang JC, Lu CW, Lin CJ. Treatment of Helicobacter pylori infection: current status and future concepts. World J Gastroenterol. 2014 May 14; 20(18):5283-93. doi: 10.3748/wjg.v20.i18.5283.
Sun Y, Zhang J. Helicobacter pylori recrudescence and its influencing factors. J Cell Mol Med. 2019 Dec; 23(12):7919-7925. doi: 10.1111/jcmm.14682. Epub 2019 Sep 19.
Tao Zhi-Hang,Han Ji-Xuan,Fang Jing-Yuan,Helicobacter pylori infection and eradication: Exploring their impacts on the gastrointestinal microbiota.[J] .Helicobacter, 2020, 25: e12754.
Algood HM, Cover TL. Helicobacter pylori persistence: an overview of interactions between H. pylori and host immune defenses. Clin Microbiol Rev. 2006 Oct; 19(4):597-613. doi: 10.1128/CMR.00006-06.
Kori M, Daugule I, Urbonas V. Helicobacter pylori and some aspects of gut microbiota in children. Helicobacter. 2018 Sep; 23 Suppl 1:e12524. doi: 10.1111/hel.12524. PMID: 30203591.
van Amsterdam K, van Vliet AH, Kusters JG, van der Ende A. Of microbe and man: determinants of Helicobacter pylori-related diseases. FEMS Microbiol Rev. 2006 Jan; 30(1):131-56.
Waskito LA, Yamaoka Y. The Story of Helicobacter pylori: Depicting Human Migrations from the Phylogeography. Adv Exp Med Biol. 2019; 1149:1-16. doi: 10.1007/5584_2019_356. PMID: 31016625.
Pereira-Marques J, Ferreira RM, Pinto-Ribeiro I, Figueiredo C. Helicobacter pylori Infection, the Gastric Microbiome and Gastric Cancer. Adv Exp Med Biol. 2019; 1149:195-210.
RU Nan, DU Yi-qi, LI Zhao-shen. Evolution of Helicobacter pylori eradication indications [J]. chinese journal of practical internal medicine, 2019, 39(006):515-519.
Helicobacter Pylori and Peptic Ulcer Group of Gastroenterology Branch of Chinese Medical Association, National Helicobacter Pylori Research Collaboration Group, Liu Wenzhong, et al. The Fifth National Consensus Report on Management of Helicobacter Pylori Infection [J]. Gastroenterology, 2017(6).